Dr Karim Brohi, trauma and vascular surgeon, an expert in trauma patients in the pre-hospital field, dedicated to focusing on how to improve primary care. His intervention in Italy during the REMOTE Congress has been very significative.
Dr Karim Brohi is a leading mind in the development of the correct path for saving trauma patients. He is the Director of the C4TS. The centre focuses on the immediate post-injury phases, with research into the pathophysiology of injury. Research is seeking for the correct pathway to ensure the translation of research into practice and policy. Dr. Brohi provided the first speech in Vergiate for the REMOTE Congress, the first meeting of which was organised by Leonardo Helicopters and SIAARTI. Dr. Brohi’s intervention focused on how to improve trauma care (primary care phase) and the outcomes of trauma patients worldwide.
Brohi is a Trauma and Vascular Surgeon with a strong academic focus on translational and clinical research into acute injury care. His trauma surgery practice is based in the Royal London Major Trauma Centre, a part of Barts Health NHS Trust and one of the busiest trauma centres in Europe, managing severely injured patients from all across metropolitan London.
So, with that, we had expected an out-of-the-box intervention during REMOTE, and we listened to a very exciting lecture about a pre-hospital trauma care approach for the air ambulance service, proposed in Italy.
“Keeping a trauma patient alive is not only a matter of time. It is also a matter of the procedure and operation that we can accomplish close to the event, in minutes and metres from the

Training for pre-hospital trauma patient assessment (source: Twitter)
accident”. Dr. Brohi focuses his intervention on a specific core: mind-changing on traumatic assessment. It’s not a matter of what you can do; it’s a matter of what your patent need, and you can attend to those needs immediately. This can change the path of the operation you arrange right from the street all the way to the Trauma Centre. The air ambulance service is an essential team you can access for saving trauma patients, and it is not merely a matter of time.
“It’s inspiring to be here in Italy for the REMOTE Congress. It’s great to see so many different prehospital providers from around the world coming together and discussing pre-hospital trauma care, and working together on how to deliver advanced care. It’s important to learn from each other about how we can build a network to develop an outstanding map of what kind of intervention is good and what type of intervention is less usable,” Dr. Brohi said in our interview.
“It’s always valuable when a national organizations produce guidelines that fit well and are backed by solid evidence-based medicine. We can discuss these guidelines, and we can define better what is the official practice that can work well on the scene”.
The first problem you highlight in your speech is that several outcomes can occur when you have trauma patients. Is there a specific path to follow?

London Air Ambulance, pioneering pre-hospital techniques on the scene (source: Express.co.uk)
“When trauma patients are injured, there are many potential outcomes: people may die in the street, they may survive, they may get into the operating room, they may die in another situation for varying reasons. What is important to understand is that all of those complications are almost set in stone, in the street, in the first few minutes after the injury. It is not just what happened or what you do in delivering prehospital care. It is what you do or what you don’t do that affects your patient. It is a big opportunity to intervene for a better outcome because what you need is a little push to change the expected result”.
What may be needed from helicopters to improve your efforts? Is it a matter of equipment? Can the air ambulance be improved for intervention in an extreme environment?
“Medical devices on helicopters are even more efficient, lighter and more robust, as well as portable. Although I think, on the other hand, you must be aware that we can’t just increase the number of the medical device onboard, without having a clear evidence-based reason for why we are carrying it. Is it efficient? If you don’t have the evidence, then your next effort between multiple different providers is to provide that evidence. Or, even better, start understanding trauma patients needs, and then develop the new equipment and the new diagnostics to help you with them”.
Transport of trauma patients – Do we have to implement a service that can reduce transport time from the point of the accident to the hospital?

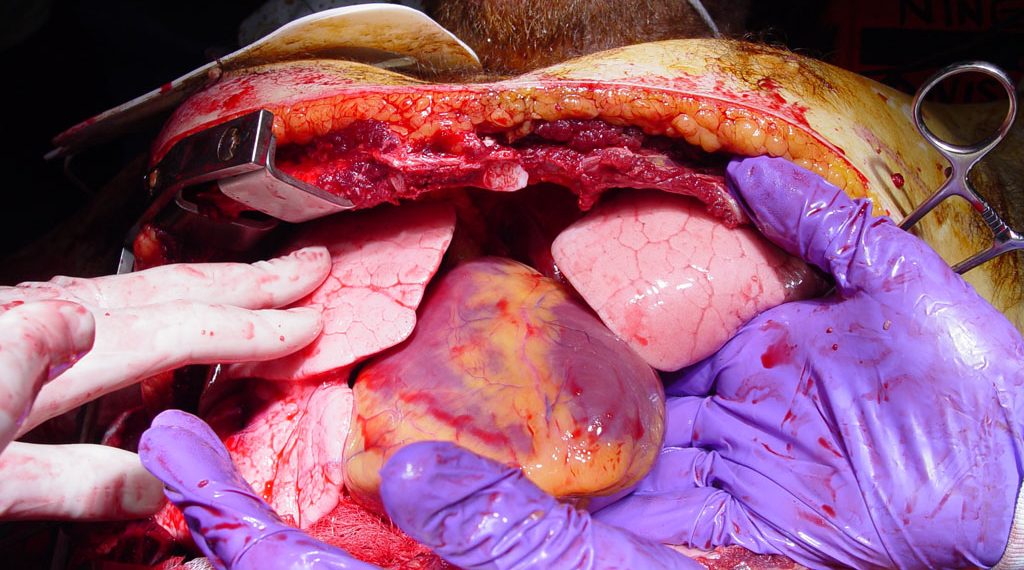
HEMS is able to perform surgery that we usually see on operating table, near to the trauma event on the accident scene. (Source: Auckland HEMS)
“No, I didn’t say that- People’s ailments develop over time, and if you save them in one place, they will get a second chance. If they die earlier, then you never see that there is a continuum. What you do in the first-minute affects the other interventions. We know now there are interventions that can improve survival on the way to the hospital, so things like giving rapid support, giving blood, avoiding crystalloids, or colloids, potentially using the tourniquets or other instruments to achieve temporary hemostasis, and then tools for brain injuries or other skills. All of these interventions have to be put in the context of the trauma patients – who is not going to stop his or her journey to the hospital.”
Is there a specific trauma patients treatment idea, or clinical philosophy, you think that HEMS will have to follow in the future?
“No. It is not the case that one professional needs to achieve one skill and then stop. It’s different; the system has to provide seamless care for the trauma patients, one step to the next. It is better to individualise your care to what each patient needs. One philosophy doesn’t achieve anything. Just as you will give the same antibiotic to everybody who comes to the hospital. There is no one thing for every patient. Some people need to move quickly; some people need to be stabilized. Understanding individual needs is a vital thing in pre-hospital trauma care“.
It seems you have a vision of pre-hospital doctors with a specific attitude, is that a necessity for selecting the best professionals to operate in the air ambulance service?
“No, A specific attitude is not required. The focus is to move away from your work being defined by the environment, to your work being defined by the trauma patients. For that reason, sharing information is so important. Some people are beginning to develop a network for pre-hospital care, and we need more cooperation between different services. There are many ways to do it; the main one is building trust between different providers to make sure that everybody is engaged, everybody feels they have ownership, and also to understand why research is crucial for trauma. So, there are a lot of different ways to do a collaboration.”
___________________________________________________
About Dr Karim Brohi