The administration of ketamine to support emergency and essential surgery when no anaesthetist is available is a very thorny matter in the medical field. In order to know more and deeply analyze this case, we interviewed dr. Sebastian Suarez Associates a global health research scientist at Massachusetts General Hospital who carried out research in Luanda Kenya about the administration of ketamine to patients.
We read a technical and specific issue you published in collaboration with other experts on an intraoperative awareness with ketamine based anesthesia in areas where it lack, in particular where anesthetists are absent like many countries of Africa and Asia. This is very interesting because the use of ketamine is still much discussed in medical field all around the world.
- What ES-ketamine stands for?
Starting by a context, in the world there are currently five billion people with no timely access to surgery so that’s about two-thirds of the world’s population and 30% of that is due to a lack of anesthesia services which which can range from a lack of anesthesia medications machines or lack of anesthetist for example in Kenya we’ve learned that there are about 0.44 anesthetists per 100,000 people and there are some areas very secluded regions of the country that have closer to 0 anesthetists per hundred thousand people so there’s a huge gap that needs to be addressed so that’s how the program ESM ketamine arose and the what it actually means of ESM is every second matters for emergency and essential surgery.
This program started in 2013 by dr. Thomas Burke here in the division of global health the human rights and how the program what ESM ketamine means is that we’ve created a training for clinicians to provide ketamine and supportive surgery when known as this is available only and specifically ketamine because this is a drug that enhances the cardiovascular system, preserves respiratory, reflexes so there’s no intubation or advanced airway management required and it’s been used for over 60 years especially in these settings and by military deployed in the field so since its inception we’ve trained approximately 200 providers in western Kenya to support surgeries particularly when no one else is available.
- Regarding this drug we suppose that will be criteria that regulates the administration, so which kind of inclusion criteria do you follow to administer ketamine on patients?
The first step that we teach the clinicians says they must try to secure an anesthetist so request that all of them call there and as it says at their facilities if there’s one available but sometimes there’s no anesthetist, but sometimes if there is they may be busy in another surgical case or they may be far away or they may be on vacation. So it’s difficult, but once we establish that no one anesthetist is available then the ESM ketamine pathway is activated on one of four different criteria.
The first one, which I believe is the most important one is when there is an emergency surgery, so for example a woman comes in with obstructed labor and needs to have a C-section but there’s no anesthetist to support the surgery so then the pathway is activated and we can give ketamine to help support the cesarean section.
The second one is when delay would compromise cares, for example a patient comes in with a fracture after having a motor vehicle accident and it’s compromising the blood supply of the limb, so they have approximately two hours before irreversible damage starts occurring. If it’ll take more than two hours to secure an anesthetist then we also activate the ketamine pathway in this case.
The third indication would be when an anesthetist would previously not have been called so in many areas of or many countries around the world there are certain conditions or procedures that are not being supported by an assitant for example manual vacuum examinations or dislocation reductions and these are very painful procedures but because of the culture and lack of historical lack of anesthesia services they’re usually not done with an anesthetist so then in this case they would also there would also be an indication for ketamine administration and then the last one is when when a patient is offered regular care but there they’re unable to financially support this care because they maybe had a family they may have they have two employments or no employment and they have to support their five children so they prefer not to have the surgery so when we then we would offer this alternative for them to be able to have care while not suffering from financial loss.
- According to your study who can administer ketamine?
Let us make a distinction first: ketamine has is a widely available drug in many countries and it’s been available for more than 60 years there’s abundant evidence that it’s effective and a safe drug given its unique properties and even some considered to be one of the safest anesthetic because it doesn’t require intubation and it’s for example it’s administered by general practitioners around the world in many countries they’re trained to provide ketamine in medical school or nursing school but our program why it’s different it’s because it’s based in a low-resource setting where these were no anesthetists or specialists were not available.
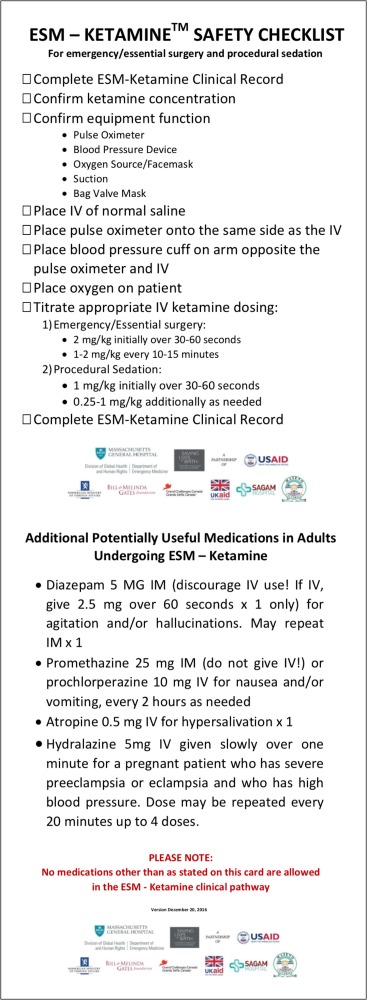
So we’re training three different types of clinicians to “fill this gap”. One of them is nurses, the other one our clinical officers, who are what we call here in the US physician assistants, and we also train medical officers who are physicians who recently graduated from medical school but are in that step before starting or pursuing more specialized training. They’re like clinician so they’re trained in the healthcare and but they’re not they don’t require that extensive training that would take years so how we designed the program is we created a checklist the pocket-size checklist that clinicians can follow it’s a very easy step-by-step process they can follow where it has the dosage to maintain those is what other medications could be administer in case there’s a side effect so it’s very easy for them to follow once they understand how it works.
- In relation to the administration of ketamine to traumatic patients, what do you think about the potential use of ketamine as a pre-hospital scenario?
I think it’s been used before and I think it’s a very adequate space to use ketamine so it’s been widely used by deployed military and I know like for example it’s been used throughout the entire military chain of evacuation from the point of injury until the point of permanent treatment. For example in the UK military are transferred from their deployment over to the UK and all this time they’re the patient is supported by ketamine also clinicians would join the army they’re giving training to use ketamine for the treatment of pain before definite of treatment. Definitely there’s a space there and it’s also very valuable situations of mass casualties for example people who are trapped under debris or under any type of structure they can receive ketamine recitation through ketamine just for pain control and sedation and that facilitates the extraction of people from these scenarios I also think about how it could be useful in the setting of motor vehicle accidents which is the main cause of injury around the world say for example someone suffers from an accident on the road and they have a fracture or at this location that’s very painful and then paramedics or whoever is helping in the clinician without being in the field can actually use ketamine to say reduce the fracture that dislocation or give sedation to maybe to intubate the patient if it’s necessary and they have the adequate training to do that. I think there’s a lot of space for ketamine in that area okay perfect and speaking about pre-hospital scenarios.
- Let’s talk about rural medicine: is ketamine a drug that can help nurses and paramedics in a country with a dominant role of rural medicine like Kenya for example?
Yes, definitely. In many low and middle-income countries ketamine is already used by many clinicians when there are no one else is available and we actually believe or the program is based on the belief that everyone deserves or has the right to a fully trained anesthetist who is capable of supporting and managing any complications that may arise from the anesthesia unfortunately training enough anethetists will take some time probably not even in her lifetime but in the nextgeneration and most of those initiatives will end up working in urban areas. There are certain countries where there’s a more dominant role of rural medicine so I think that training other clinicians to administer ketamine as an interim solution until there are enough an asset is to provide those services it would be a huge help just to increase access to surgeries or procedures that would not have been able to perform.
- Are you working for the diffusion of the ESM K protocol in your emergency and in the prospect of emergency settings?
Yes, the ESM ketamine program is particularly important in emergency settings as I mentioned. The program actually arose or started to support C-sections to reduce maternal and infant mortality. Even though it started in these emergency situations the trained clinicians actually adopted the protocol and expanded its use to include the use ketamine in or painful procedures such as a reduction of fractures or dislocations which do not necessarily require offer of an operating theater but maybe just in the emergency setting and to your second question in a pre-hospital emergency settings even though I talked about a little bit about the like previous knowledge on its use in this setting and I do believe that there’s a there’s a role for ketamine in this setting our program is still considered a research study so we’re still we’re not currently looking to expand it to the pre-hospital emergency setting first we’re trying to ensure that the benefit actually outweighs the harm before we scale up to other settings because even though it’s been widely used there’s there no actual like let’s say randomized trials or anything like that but sirs we’re trying to build up the evidence to make sure that this is something that should be scaled up but having said that I think it’s definitely something to think about in the future and how to increase its its support for other settings.
- Are you satisfied with the results you have obtained this far?
We’re very satisfied with the results so far I think part of the success is that we partnered with the county and national ministries of health and they’ve supported the program so we have a lot of support in Kenya and we also have a strong relationships with the local stakeholders, local physicians, local champions. Actually the training is performed by local anesthetist and trainers and so we’re just here to support them and they’ve been I think part of the successes, because they owned the the program and we’ve given that space of ownership for them and I also think it’s been possible to where funders which are the Elrah’s research for health and humanitarian crises or our cheap program and the saving lives at birth partners which are USAD, Government of Norway, the Bill and Melinda Gates Foundation that are Grand Challenges Canada, the UK government, Korean International Corporation. Different organization supporting this and I think having that up back up has been very important for the for the success and results that we’ve been able to obtain and I think now we’re in the process of scaling up to other regions in Kenya including counties that are considered to be in a humanitarian crisis because of refugees coming in from other countries neighbouring countries and this is what we’re trying to move towards and naturally expanding the program to ultimately increase the timely access to surgery of to underserved communities and by doing so achieving universal health coverage which is one of the priorities in Kenya bright now.
LISTEN TO THE PODCAST