EVALUATION OF SERUM NEURAL SPECIFIC ENOLASE DURING THE FIRST 72 HOURS AFTER ICU ADMISSION AS A PROGNOSTIC INDICATOR IN POST-CARDIAC ARREST SYNDROME
Authors:
Giovanni Babini 1
Salvatore Alongi 2
Alberto Sicignano 2
Antonio Pesenti 1,2
1 Department of Pathophysiology and Transplantation, University of Milan, Milan, Italy.
2 Department of Anesthesia, Critical Care and Emergency, Fondazione IRCCS Ca’ Granda Ospedale Maggiore Policlinico, Milan, Italy.


Emergency Live is pleased to announce the collaboration with IRC-Italian Resuscitation Council. On EMSpedia we will re-launch posters and scientific publication from the last National Congress.
Remember that in 2018 the European Resuscitation Council Congress will be hosted in Italy, Bologna, from 20 to 22 september
Background. Serum neural specific enolase (NSE) is a biomarker currently used to define the extent of neurological injury in patients that are successfully resuscitated from cardiac arrest. NSE over 33 µg/l at 48-72 h from intensive care unit (ICU) admission has been proposed as a negative prognostic indicator.[1] However, since the introduction of temperature control, this cut-off value demonstrated conflicting results.[2,3] For this reason, current guidelines recommend using NSE serum concentrations in prognostication after CA but do not recommend a specific threshold.[4] Modification over time of serum NSE may be associated with an higher sensitivity and specificity in this cohort of patients, and it may potentially enhance the predictive power of this biomarker.
Objective. To evaluate the reliability of NSE absolute value and its modification over time during the first 72 h from ICU admission as a prognostic indicator in patient resuscitated from cardiac arrest. In this preliminary analysis the outcome evaluated was survival to ICU discharge.
Material and methods. We retrospectively collected in-hospital data from cardiac arrest patients admitted in ICU from November 2012 to August 2017. All serum NSE values collected during the first 72 h from ICU admissions were included in our analysis. Patients that died before 72 h from ICU admission and those with no NSE data were excluded from further analysis.
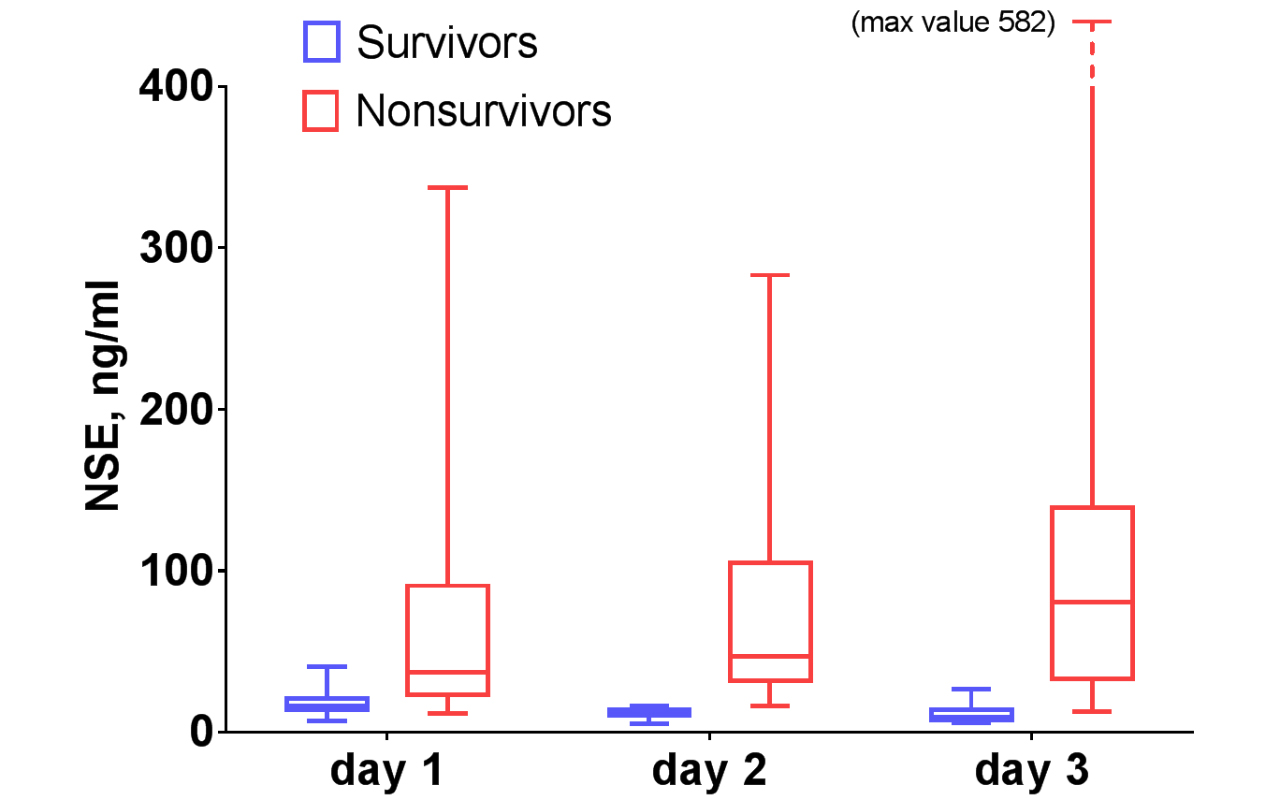
Results. We included 79 patients in our analysis and 27% survived to ICU discharge. Forty-five patients (57%) were treated with temperature control between 33 and 36°C. We collected a total of 38 NSE values at day 1, 32 values at day 2 and 37 values at day 3. In survivors median NSE values was 15.9 [13.9;21.0] µg/l at day 1, 11.5 [10.2;13.8] µg/l at day 2 and 9.1 [7.2;13.8] µg/l at day 3, showing a significant reduction along the first 72 h from admission (p = .05), particularly between day 1 and day 3 (p < .05)(figure). Patients who died in ICU have a median NSE values of 37.1 [23.3;90.6] µg/l at day 1, 47.0 [31.6;105.0] µg/l at day 2 and 80.5 [32.9;139.0] µg/l at day 3; the increase in NSE values was not significant, however we observed a significant difference between day 1 and day 3 (p = .03)(figure). The difference in absolute median NSE values between survived and deceased patients was significant at each time point analyzed. This data confirmed the results observed in previous studies.[5,6]
In survivors, mean percentage difference in NSE serum level was -18.7 ± 24.4 % from day 1 to day 2, -17.7 ± 24.3 % from day 2 to day 3 and -22.2 ± 36.0 % from day 1 to day 3 (p not significant). Patients who died had a mean percentage difference in NSE serum level of 65.9 ± 114.0 % from day 1 to day 2, 31.6 ± 61.0 % from day 2 to day 3 and 182.0 ± 252.0 % from day 1 to day 3 (p = .03). The mean percentage difference in NSE values between survived and deceased patients was significant at each time point analyzed.
We computed the sensibility, specificity, negative predictive value and positive predictive value of various NSE criteria for negative outcome reported in previous studies (table).[1,6,7] Both > 33 µg/l and > 75 µg/l threshold demonstrated good specificity and positive predictive value during the first three days of ICU admission. The increase in NSE serum concentration between day 1 and day 3 showed the best compromise in terms of sensibility and specificity (AUC 0.85±0.08, p<0.01), whereas an increase between day 2 and day 3 was associated with the higher specificity and positive predictive value (table).
Conclusion. Serial measurement of serum NSE during the first 72 h from ICU admission could be useful in identify cardiac arrest patients that would die before ICU discharge. Furthermore, our data showed that an increase in serum NSE concentrations during the first 72 h from ICU admission, particularly from day 1 to day 3, is a good indicator of bad outcome. Further studies are needed to confirm this preliminary results, particularly on long term outcomes.
References
1.Wijdicks EF, Hijdra A, Young GB, et al; Quality Standards Subcommittee of the American Academy of Neurology: Practice parameter: Prediction of outcome in comatose survivors after cardiopulmonary resuscitation (an evidence-based review): Report of the Quality Standards Subcommittee of the American Academy of Neurology. Neurology 2006; 67:203–210
- Zellner T, Gärtner R, Schopohl J, Angstwurm M. Clinical paper NSE and S-100B are not sufficiently predictive of neurologic outcome after therapeutic hypothermia for cardiac arrest ଝ. Resuscitation European Resuscitation Council, American Heart Association, Inc., and International Liaison Committee on Resuscitation. Resuscitation, 2013;84:1382–6.
- Huntgeburth M, Adler C, Rosenkranz S, et al. Changes in neuron-specific enolase are more suitable than its absolute serum levels for the prediction of neurologic outcome in hypothermia-treated patients with out-of-hospital cardiac arrest. Neurocritical Care 2014;20:358–66.
- Sandroni C, Cariou A, Cavallaro F, et al: Prognostication in comatose survivors of cardiac arrest: An advisory statement from the European Resuscitation Council and the European Society of Intensive Care Medicine. Resuscitation 2014; 85:1779–89
- Stammet P, Collignon O, Hassager C, P Wise M, Hovdenes J, Åneman A, et al. Neuron-Specific Enolase as a Predictor of Death or Poor Neurological Outcome After Out-of-Hospital Cardiac Arrest and Targeted Temperature Management at 33°C and 36°C. Journal of the American College of Cardiology 2015 ;65:2104–14
- Wiberg S, Hassager C, Stammet P, Winther Jensen M, Thomsen JH, Erlinge D, et al. (2017) Single versus Serial Measurements of Neuron Specific Enolase and Prediction of Poor Neurological Outcome in Persistently Unconscious Patients after Out-Of-Hospital Cardiac Arrest – A TTM-Trial Substudy. PLoS ONE 12(1): e0168894. doi:10.1371/journal.pone.0168894
- Oddo M, Rossetti AO. Early multimodal outcome prediction after cardiac arrest in patients treated with hypothermia. Critical Care Med 2014;42: 1340–7
 Table
Table
| Sn, % | Sp, % | NPV, % | PPV, % | P value | |
| NSE > 33 ng/ml
day 1 day 2 day 3 |
56 70 76 |
91 100 100 |
45 56 67 |
94 100 100 |
0.01 <0.01 <0.01 |
| NSE > 75 ng/ml
day 1 day 2 day 3 |
26 30 54 |
100 100 100 |
31 36 52 |
100 100 100 |
0.16 0.15 <0.01 |
| Positive Δ NSE
day 1 → 2 day 2 → 3 day 1 → 3 |
60 75 81 |
75 88 80 |
50 64 73 |
82 92 87 |
0.19 <0.01 <0.01 |

