Authors: Stella M., Pellis T., Marchesini F., Roman Pognuz E.
From: “Università degli Studi di Trieste” and “Ordine dei Medici Chirurghi e Odontoiatri della Provincia di Pordenone”
INTRODUCTION
The province of Pordenone (a north-east region of Italy) has a population of 290,229 people distributed in an area of 2273 km2. In 2012 the number of confirmed out-of-hospital cardiac arrests (OHCA) in this area was 425, with a prevalence of 1.46 per 1000 inhabitants. Comparing some data of 1994 and 2003 most of these OHCA occurred at home (64% and 78%), in some cases they occured in the ambulance during the transport to the hospital (3% and 9%) and the remaining cases in public places (13% and 33%). Among public places, General Practitioners and Pediatric clinics, Dental surgeries and all the other medical facilities distributed in the territory, represent important aggregation centers for people with diseases and risk factors for cardiac
arrest (CA).
Therefore the “extra-hospital” doctors’ skills and the presence of all the necessary devices to treat OHCA (i.e. defibrillator, drugs and ventilation devices) become fundamental. Studies have shown that early recognition of CA and immediate cardio-pulmonary resuscitation (CPR) performed by bystanders can double or quadruple the survival from CA. Chest compressions and early defibrillation are the major determinants of survival from OHCA.
Defibrillation within the first 3-5 minutes after a CA can increase survival up to 50-70%. Many studies show that CPR skills are reduced within three and six months from the initial training.
OBJECTIVE
The aim of this study is to evaluate the out-of-hospital doctors skills to manage an OHCA. We investigated the presence of devices in the clinics distributed in the territory and the preparation/propensity of the doctors regarding this topic.
METHODS
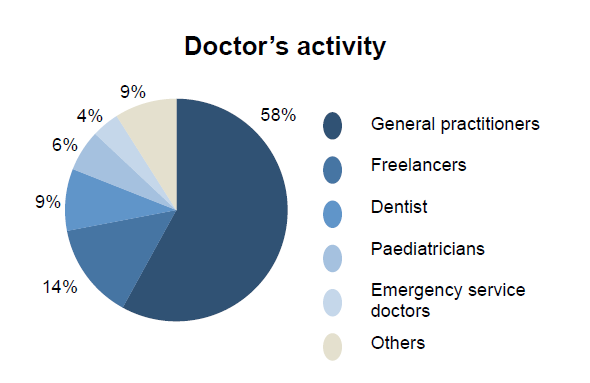
A questionnaire with 23 closed-ended questions was drawn up and distributed by e-mail since October until November 2015. The participants of this study were doctors enrolled in the Order of Physicians of the city of Pordenone, who were under 75 years old, working in the territory outside of hospitals (general practitioners, paediatricians, dentists, freelancers and emergency service doctors.
RESULTS
298 doctors participated and were considered for this study. More than half (58%) of the interviewees worked as general practitioners (GPs) so they had an important weight in the results of this study. Most of the doctors involved (59%), had a long working experience since they had graduated before 1990. 62% of them worked in one clinic only, while the remaining 38% worked in several clinics.
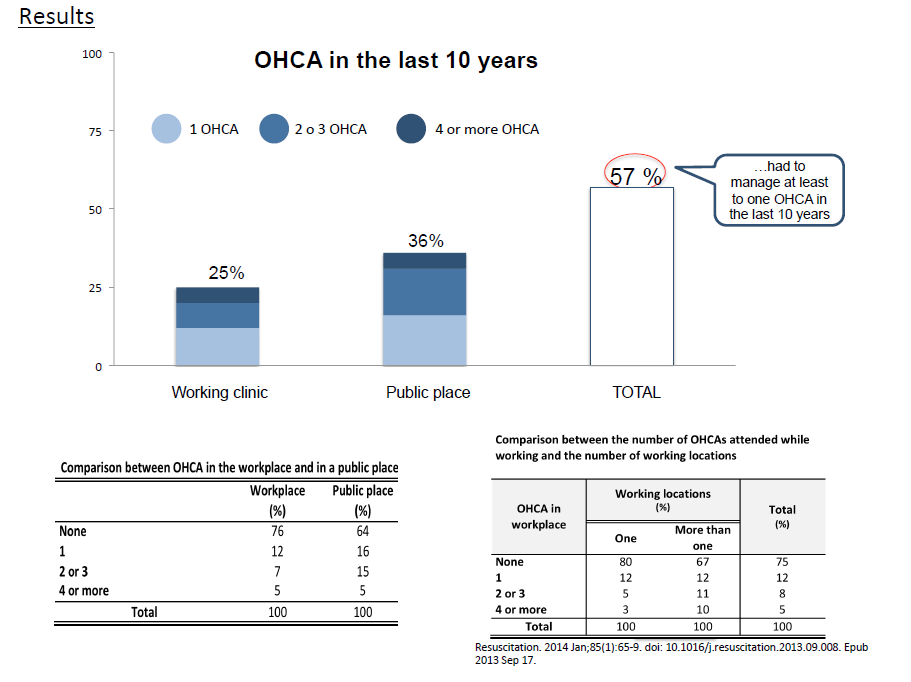
25% of the interviewed doctors attended at least to one CA while working in their clinic and 36% attended at least to one in a public place, as civilian. Without considering the place of the event, 57% of all respondents had to manage at least one CA in the last 10 years.
According to literature, physicians working in multiple locations have attended to more CAs (33%) than those working in a single clinic during the last 10 years (20%), a difference which is statistically significant (pvalue <0.05).
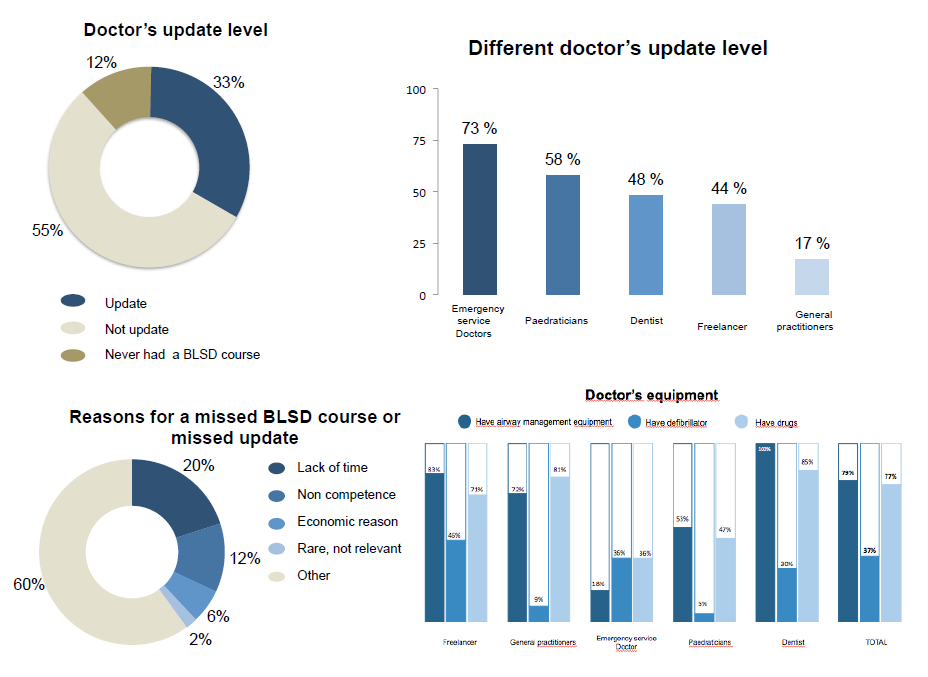
33% of respondents were trained to manage CAs having recently participated in a BLSD course or to an update of it recently (within 2 years). About 55% have attended to a BLSD corse in the past years (more than 2 years) resulting as not updated and the remaining 12% have never participated to a BLSD course.
Most up-to-date doctors, in our study, were emergency service doctors (73%) followed by paediatricians (58%), dentists (48%), freelancers (44%) and lastly general practitioners (17%). The reasons for a missed BLSD course or missed update are not well identifiable, considering that 60% of the not updated doctors did not give a clear answer. Someone identified the lack of time (20%) as a cause, others the “non-competence” (14%) considering the OHCA problem not relevant for the out of hospital doctors and lastly the cost of the courses (6%).
79% of the respondents had airway management equipment (bag-valve-masks or pocket masks) in their clinic, 37% had defibrillator and 77% had medications to treat an OHCA (adrenaline and / or amiodarone ). The best equipped were the freelancers, followed by dentists, general practitioners and paediatricians and finally the emergency service doctors.
The reasons for the absence of devices, according to the interviewees were related to two main factors. First of all the economic burden (28%), due to the high cost of the devices, especially the defibrillator. The second reason was that the OHCA figured as an underestimated problem. Specifically, 23% believed that the emergency network is quick and effective in their interventions, 9% believed that OHCAs are so rare that providing tools and knowledge is not necessary and another 5% said that even if they had the devices, they would not be able to use it. Comparing the data about the presence of the various devices and the level of update, it can be noted that doctors who are not updated on the BLSD were also less supplied in materials and therefore less ready to manage a possible OHCA.
Investigating the respondent’s conduct during an OHCA, it was possible to observe that 20% of the updated doctors managed and performed both the CPR and the defibrillation whereas only 2% of the non-updated doctors.
The last part of the questionnaire was intended to investigate the perception of the problem by the interviewees and their inclination/ need for courses or updates. There is a correlation (correlation index = 0.24) between the level of update (and the familiarity with the maneuvers of the BLSD acquired in the courses) and the ability to manage an OHCA. However, as previously highlighted, even in this phase of the analysis about the ability to manage an OHCA, a part of respondents (42%) showed to probably underestimate the problem of the CA declaring to have enough or a lot of ability to handle it, even if they were not updated or never had a BLSD course.
The importance of the BLSD course (and related updates) is also emonstrated by the answers to the question that investigated the aspects of greater insecurity or “fear” performing CPR execution. The majority (66%), in fact, claimed “lack of experience” about the proper execution and timing of the maneuvers. 85% of the interviewees attributed a higher level of responsibility
to the doctor’s action compared to civilians in managing a CA in public places. 95% of doctors expressed the need of more training, but despite this the contrast with the percentage of updated doctors among those interviewed, remains rather low (33%), which shows how the problem is currently underestimated .
CONCLUSIONS
According to our data, OHCA cannot be considered a rare and non-pertinent event for out-ofhospital doctors. Despite this, up to date doctors, defibrillators, drugs and devices distribution, were significantly lower than the real needs in the extra-hospital environment. The relevance of BLSD courses and the importance of continuous updating emerges in several points. In our study, updated doctors were more able and more equipped with devices to manage an OHCA than the not updated doctors.